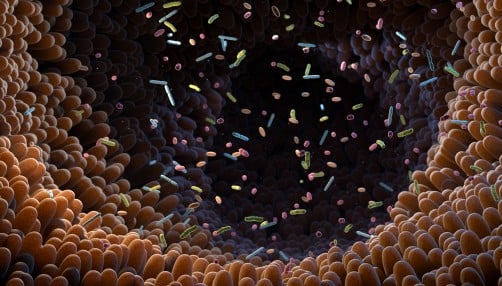
BREAKING: A groundbreaking study from UCLA Health reveals that a child’s early gut microbiome could be a critical factor in their risk of developing anxiety and depression later in childhood. This urgent finding, published today in Nature Communications, highlights that children with higher levels of specific gut bacteria are at increased risk of experiencing internalizing symptoms, such as depression and anxiety, by age 7.5 years.
Researchers discovered that the gut microbiome of children at age 2 years, specifically those with a high representation of bacteria in the Clostridiales order and Lachnospiraceae family, showed significant correlations with emotional health outcomes. The study’s senior author, Dr. Bridget Callaghan, emphasizes that this connection operates through altered communication in emotion-related brain networks, potentially programming brain circuits tied to emotional well-being during crucial developmental years.
This observational study utilized data from the Growing Up in Singapore Towards Healthy Outcomes (GUSTO) project, which collected extensive health information, including stool samples from children at age 2, brain scans at age 6, and behavioral assessments from caregivers. The analysis focused on 55 participants and sought to determine how early gut microbiome composition could influence mental health as children grow.
Dr. Callaghan noted the significance of these findings: “By linking early-life microbiome patterns with brain connectivity and later symptoms of anxiety and depression, our study provides early evidence that gut microbes could help shape mental health during the critical school-age years.” This could have profound implications for understanding and addressing mental health challenges as children transition into adolescence and beyond.
Previous research primarily focused on infants and toddlers, often overlooking school-aged children. This new investigation opens the door for further studies on how gut health influences emotional development and mental health risk factors. The researchers are now exploring whether specific microbial species within the identified groups are driving these associations.
Dr. Callaghan urges the need for future experimental research to determine causality, stating, “Once we have that information, there are relatively straightforward ways to change the microbiome, like probiotics or diet, that we could use to address issues.” The study also included contributions from Drs. Francesca Querdasi and Jessica Uy, with the collaboration of institutions such as KK Women’s and Children’s Hospital and the National University of Singapore.
As mental health issues continue to rise among children, this urgent research underscores the potential of early interventions targeting gut health. Parents, caregivers, and health professionals should be aware of these findings and consider the implications for children’s emotional well-being.
Stay tuned for updates as researchers delve deeper into the gut-brain connection and its impact on childhood mental health. This study may pave the way for innovative strategies to enhance emotional resilience in young children worldwide.