In a remarkable advancement in cancer treatment, scientists at the University of California, San Francisco (UCSF) have developed a method to convert ordinary fat cells into powerful agents that can starve tumors of essential nutrients. This innovative approach, outlined in a study published on February 4, 2024, in Nature Biotechnology, utilizes genetically engineered white fat cells that act similarly to energy-burning “beige” fat. By repurposing adipose tissue, researchers aim to combat various cancer types, including breast, prostate, and colon cancers.
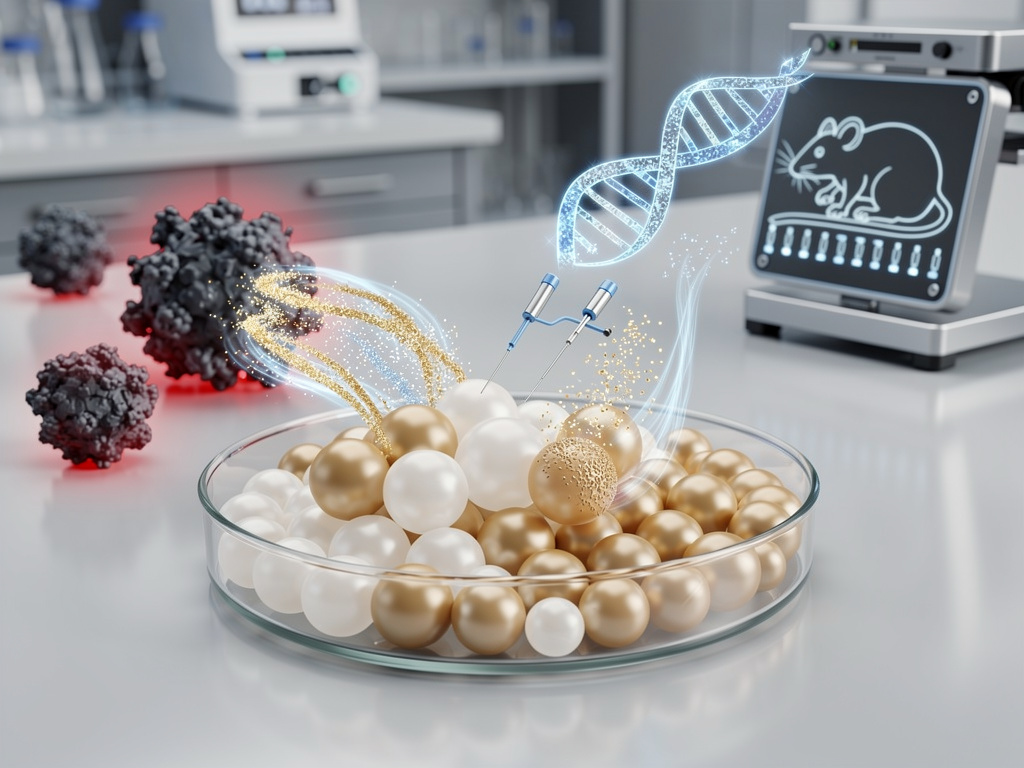
The research team, led by Nadav Ahituv, a professor in the Department of Bioengineering and Therapeutic Sciences, effectively harnesses the metabolic characteristics of fat cells to inhibit tumor growth. By using CRISPR gene-editing technology, they activated specific genes that transform white fat into highly active beige fat. In preclinical models, these engineered cells were implanted near tumors in mice, where they aggressively absorbed surrounding nutrients such as glucose, leaving little for the cancer cells to exploit.
Early results have been striking, showing tumor reductions of up to 80% and, in some cases, complete eradication without damaging healthy tissues. This targeted mechanism is a significant advantage over traditional therapies like chemotherapy and radiation, which often have severe side effects. According to the findings, the fat cells focus on local nutrient depletion, minimizing systemic disruption.
Innovative Origins and Mechanism
The genesis of this research stems from techniques in plastic surgery, particularly the use of fat grafts for reconstructive purposes. Researchers recognized the potential of these fat cells to be transformed into a competitive force against tumors. Electron microscopy from UCSF revealed that the engineered fat organoids significantly outperformed tumors in nutrient absorption, demonstrating a clear advantage in controlling their growth.
Past attempts to starve cancer cells through metabolic means have primarily involved drug therapies targeting glucose uptake or fatty acid synthesis. These methods often fail due to the body’s compensatory responses. The UCSF approach circumvents these challenges by introducing a direct competitor for nutrients. In studies conducted by the National Cancer Institute, engineered fat cells showed profound effects, reducing tumor sizes and notably extending survival rates among test subjects.
Industry experts underscore the scalability of this therapy, given that fat cells are abundant and can be harvested through minimally invasive procedures. However, challenges remain, particularly regarding the potential for engineered cells to migrate or cause unintended metabolic disturbances. Ahituv’s team is now focusing on refining these gene edits for future human applications.
Future Directions and Implications
As this innovative therapy progresses toward clinical trials, regulatory bodies, including the U.S. Food and Drug Administration (FDA), will evaluate its safety and efficacy. Concerns surrounding CRISPR’s off-target effects have been addressed by Ahituv’s team, which reports high specificity in their models. Ongoing funding from the National Institutes of Health supports further research and potential combinations with immunotherapies.
Public reactions on social media platforms reflect a mix of excitement and caution, with some users celebrating the breakthrough while others highlight the need for additional verification. While this approach shows promise, experts caution that it is not a panacea for cancer treatment. The pharmaceutical industry is closely monitoring these developments, as successful human trials could significantly impact the $200 billion oncology market.
The vision for integrating this fat-cell strategy into existing cancer treatments is expansive. Potential applications include using post-surgical fat implants to prevent cancer recurrence or injecting engineered cells to target tumors in hard-to-reach areas. This pioneering research not only positions UCSF as a leader in cancer innovation but also opens doors for additional applications in treating other nutrient-dependent diseases.
As researchers continue to refine their approach, collaborations with institutions like the National Cancer Institute are expected to expedite the translation of these findings into clinical practice. The ultimate goal is to transform fat, traditionally viewed as a health risk, into a vital ally in the fight against cancer.