Scientists at Stanford Medicine have identified the biological mechanisms behind the rare occurrence of heart inflammation, known as myocarditis, linked to mRNA COVID-19 vaccines. This discovery sheds light on how these vaccines can provoke an immune response that affects the heart, particularly in young males. Their research also suggests potential strategies to mitigate this risk.
In a study published on December 10, 2025, in the journal *Science Translational Medicine*, the Stanford team explored the immune responses triggered by mRNA vaccines. They uncovered a two-step reaction wherein the vaccine activates one type of immune cell, leading to inflammation that can cause temporary injury to heart muscle cells. This process predominantly affects adolescent and young adult males, with incidence rates of myocarditis reported at approximately one in 140,000 after the first vaccine dose and escalating to one in 32,000 following the second dose.
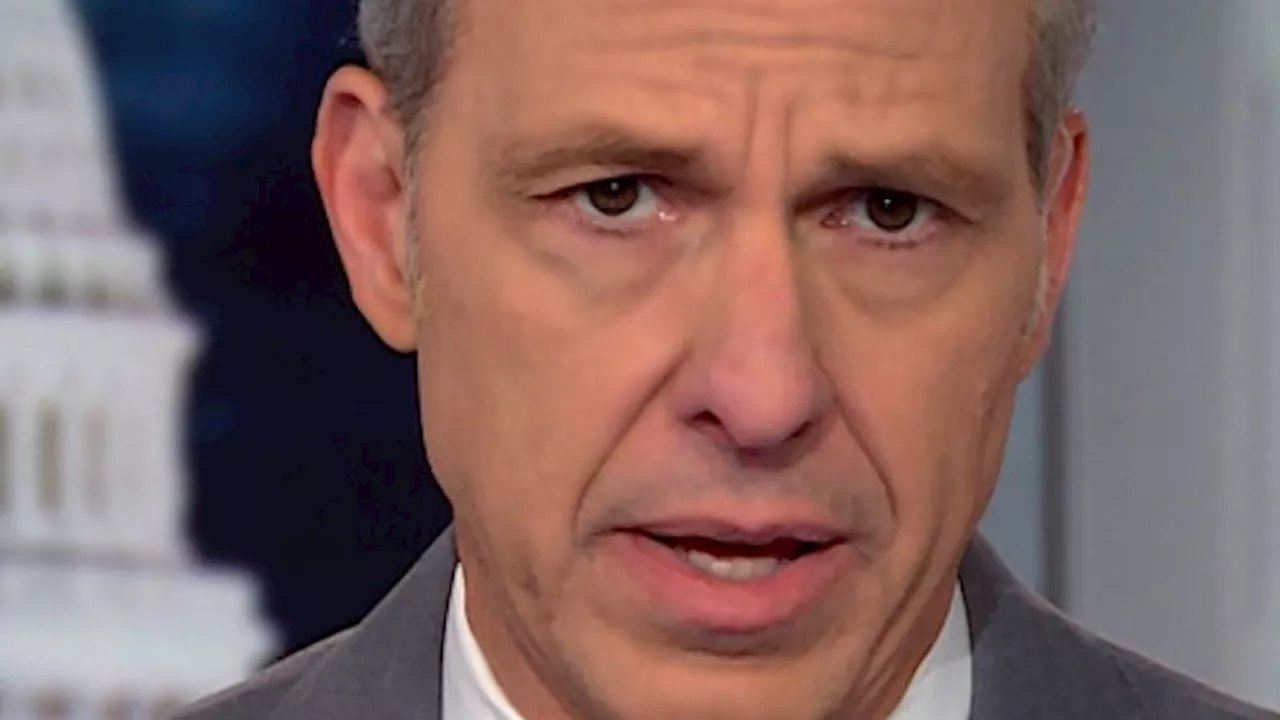
Despite these findings, the overall safety profile of mRNA COVID-19 vaccines remains robust. According to Joseph Wu, MD, PhD, director of the Stanford Cardiovascular Institute, “The mRNA vaccines have done a tremendous job mitigating the COVID pandemic.” Wu emphasized that the benefits of vaccination far outweigh the risks associated with rare side effects like myocarditis, which can occur without prior viral infection.
Understanding the Mechanism of Myocarditis
Myocarditis is characterized by inflammation of the heart muscle, with symptoms often presenting within one to three days post-vaccination. Common symptoms include chest pain, shortness of breath, and heart palpitations, typically indicating elevated levels of cardiac troponin, a marker for heart injury. Most cases resolve quickly with appropriate monitoring, and severe outcomes remain uncommon. Wu noted that a COVID-19 infection poses a significantly higher risk for myocarditis, being approximately ten times more likely to result in the condition than the vaccine itself.
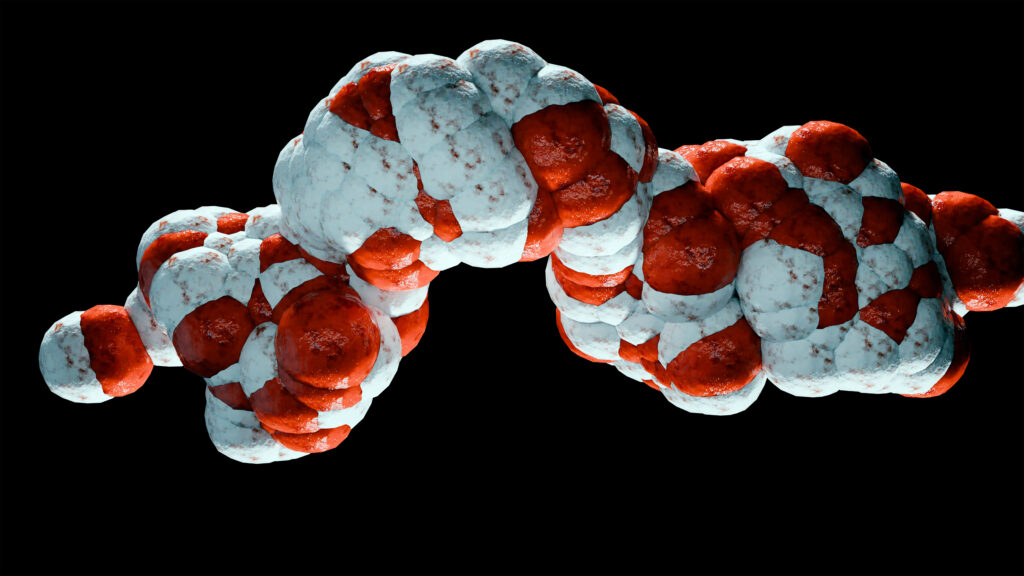
The researchers utilized a combination of laboratory techniques and clinical data to analyze blood samples from vaccinated individuals, including those who experienced myocarditis. They identified two key proteins, CXCL10 and IFN-gamma, as central to the inflammatory response. Both are cytokines, which are crucial for immune communication and regulation.
Immune Response Dynamics
To investigate how these proteins contribute to heart inflammation, the researchers exposed human immune cells called macrophages to mRNA vaccines. Upon exposure, these macrophages released various cytokines, notably elevated levels of CXCL10. The presence of T cells further amplified the production of IFN-gamma, indicating that macrophages and T cells play distinct yet interconnected roles in the immune response to vaccination.
In animal studies, young male mice vaccinated with mRNA vaccines demonstrated increased cardiac troponin levels, indicating heart muscle injury. Additionally, there was notable infiltration of immune cells into heart tissue, mirroring the immune response seen in human cases of myocarditis post-vaccination. The team found that blocking CXCL10 and IFN-gamma significantly reduced both immune cell infiltration and heart damage.
Exploring Protective Strategies
Wu’s research team also investigated potential protective measures against vaccine-induced myocarditis. They revisited genistein, a soy-derived compound with known anti-inflammatory properties. Previous studies indicated that genistein could mitigate inflammation and cellular damage in various tissues. When administered prior to vaccination, genistein effectively reduced heart damage in both cellular models and in live mice.
Wu highlighted that while mRNA vaccines are a breakthrough in immunology due to their rapid development and adaptability, they can elicit varied responses among individuals. The implications of their findings extend beyond COVID-19, as heightened cytokine activity could affect responses to other vaccines and medical interventions.
Future Research Directions
The study, supported by the National Institutes of Health and the Gootter-Jensen Foundation, opens avenues for further investigation into the effects of mRNA vaccines on heart health and beyond. Understanding the nuances of the immune response may lead to enhanced strategies for both vaccine safety and efficacy.
As the scientific community continues to evaluate vaccine impacts, Wu urges a balanced perspective on the risks associated with vaccination versus the dangers posed by COVID-19 itself. “If you get chest pains from a COVID vaccine, you go to the hospital to get checked out,” he noted, emphasizing the importance of awareness and monitoring in managing vaccine-related side effects.
In conclusion, while the findings regarding myocarditis linked to mRNA vaccines warrant attention, they also reinforce the critical role these vaccines play in combating the ongoing pandemic. Continued research and open dialogue will be essential in ensuring public confidence in vaccination efforts worldwide.