Healthcare financial leaders face an increasingly complex environment, characterized by rising operational costs and high claim denial rates. According to industry data, over 10% of submitted claims are denied, representing a significant challenge for organizations relying on manual, outdated Revenue Cycle Management (RCM) systems. This dependence exposes them to ongoing fiscal vulnerabilities that can hinder clinical innovation and patient care.
Manual RCM workflows create operational inefficiencies that can lead to major financial setbacks. The issues include data vulnerability, where errors at the point of patient registration propagate through the system, triggering denials. Additionally, skilled staff often find themselves in a reactive cycle of correcting errors and submitting appeals, exacerbating burnout and retention challenges. Furthermore, unpredictable cash flows and lack of clear denial analytics make accurate financial forecasting difficult.
AI as a Catalyst for RCM Transformation
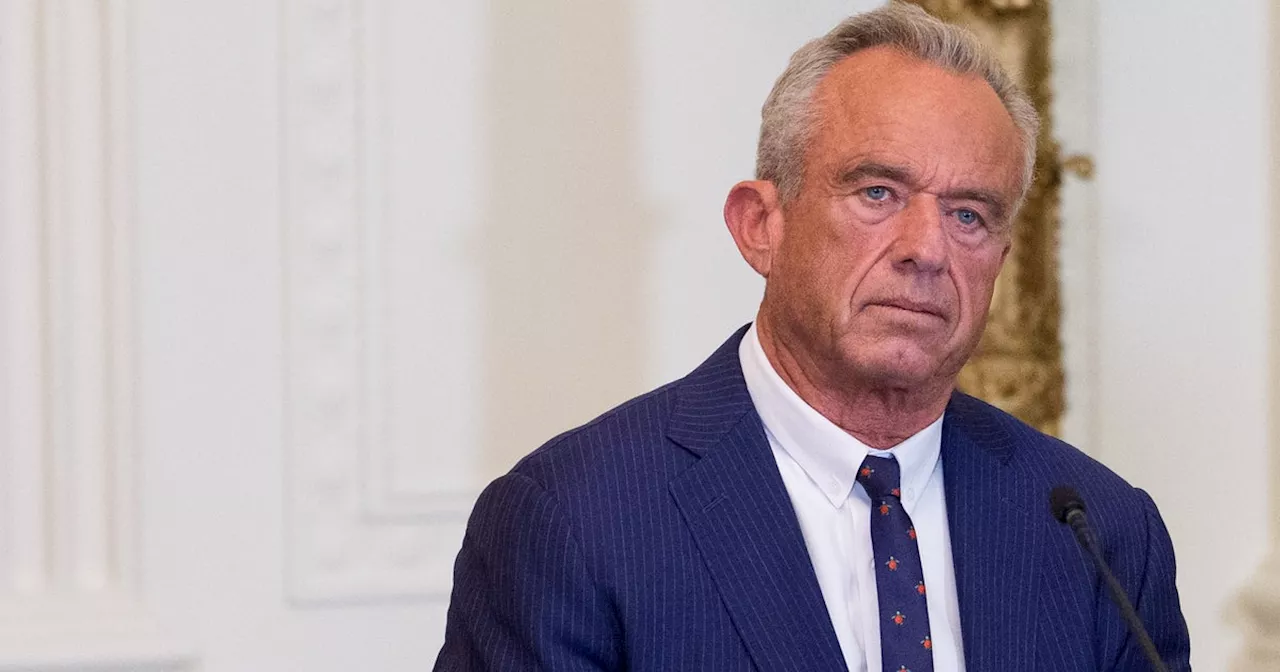
Modernizing RCM through intelligent automation is essential for ensuring long-term financial viability. Inger Sivanthi, Chief Executive Officer of Droidal, emphasizes that leveraging artificial intelligence (AI) can transform RCM from a reactive cost center into a proactive revenue engine. AI technologies, including Machine Learning (ML), Natural Language Processing (NLP), and Generative AI, can effectively handle high-volume transactions and analytical tasks, allowing RCM experts to focus on complex appeals and patient advocacy.
Organizations that strategically implement AI for claims optimization have significantly reduced denial rates by up to 40%. This reduction not only improves operating margins but also delivers a direct return on investment (ROI).
Four Key Areas of AI-Driven RCM Optimization
AI can address critical friction points within the revenue cycle, establishing systematic control and minimizing risk.
The first area is data integrity and predictive eligibility. AI can effectively eliminate the primary cause of denials—poor front-end data—by providing real-time eligibility and policy verification. By querying complex payer data instantly, AI ensures a “clean claim” foundation from the outset of patient interactions.
The second area involves accelerating prior authorization throughput. The prior authorization process is often a significant bottleneck, consuming valuable resources. AI can analyze clinical notes and payer requirements to automatically assemble necessary documentation, drastically reducing administrative turnaround time and increasing first-pass approval rates.
The third area focuses on autonomous claims quality assurance. To build a predictable revenue stream, claims must be submitted error-free. AI employs machine learning to audit every claim element, ensuring that claims meet the necessary documentation and coding standards, which can lead to a clean claim rate of 95%.
Finally, proactive denial management and prevention transform RCM by shifting from a reactive to a predictive intelligence system. AI analyzes historical data to identify patterns in denials and flags high-risk claims before submission, allowing organizations to address underlying issues rather than merely correcting individual claims.
Integrating AI into RCM is not merely a cost; it is a strategic investment in institutional resilience. When organizations adopt AI, they achieve critical outcomes: financial certainty through reduced claim denials, staff empowerment as burdensome tasks are automated, and enhanced patient trust due to accurate, timely billing practices.
As the financial landscape of healthcare continues to evolve, organizations that delay RCM modernization risk falling behind. Embracing AI is crucial for securing financial stability and refocusing efforts on delivering exceptional clinical outcomes.
About Inger Sivanthi: As the CEO of Droidal, Inger Sivanthi has played a pivotal role in advancing AI services for healthcare revenue cycles. With expertise in large language models and applied AI, he has facilitated over $250 million in cost savings for healthcare organizations through intelligent automation. His focus remains on promoting responsible and ethical AI adoption to enhance healthcare and financial outcomes on a large scale.