Influenza activity remains low in many regions of the United States, despite reports of increased sniffles and coughs. According to the U.S. Centers for Disease Control and Prevention (CDC), as of last week, flu activity was classified as high in four states: Colorado, Louisiana, New Jersey, and New York. The overall severity indicators suggest a “mild” season thus far, although health experts are expressing concerns about potential future impacts.
Winter months typically see a rise in respiratory illnesses, driven by increased indoor gatherings that facilitate the spread of viruses. In addition to influenza, health officials are closely monitoring norovirus, which has shown an upward trend in cases over the past month.
Flu Activity and Concerns for the Upcoming Months
Last season marked one of the most severe flu outbreaks in recent years, with hospitalization rates reaching their highest levels since the H1N1 pandemic of 2009. The CDC reported that child flu deaths totaled 288, matching figures from the 2009-2010 flu pandemic. This season has already seen its first pediatric flu death, raising alarms among health officials.
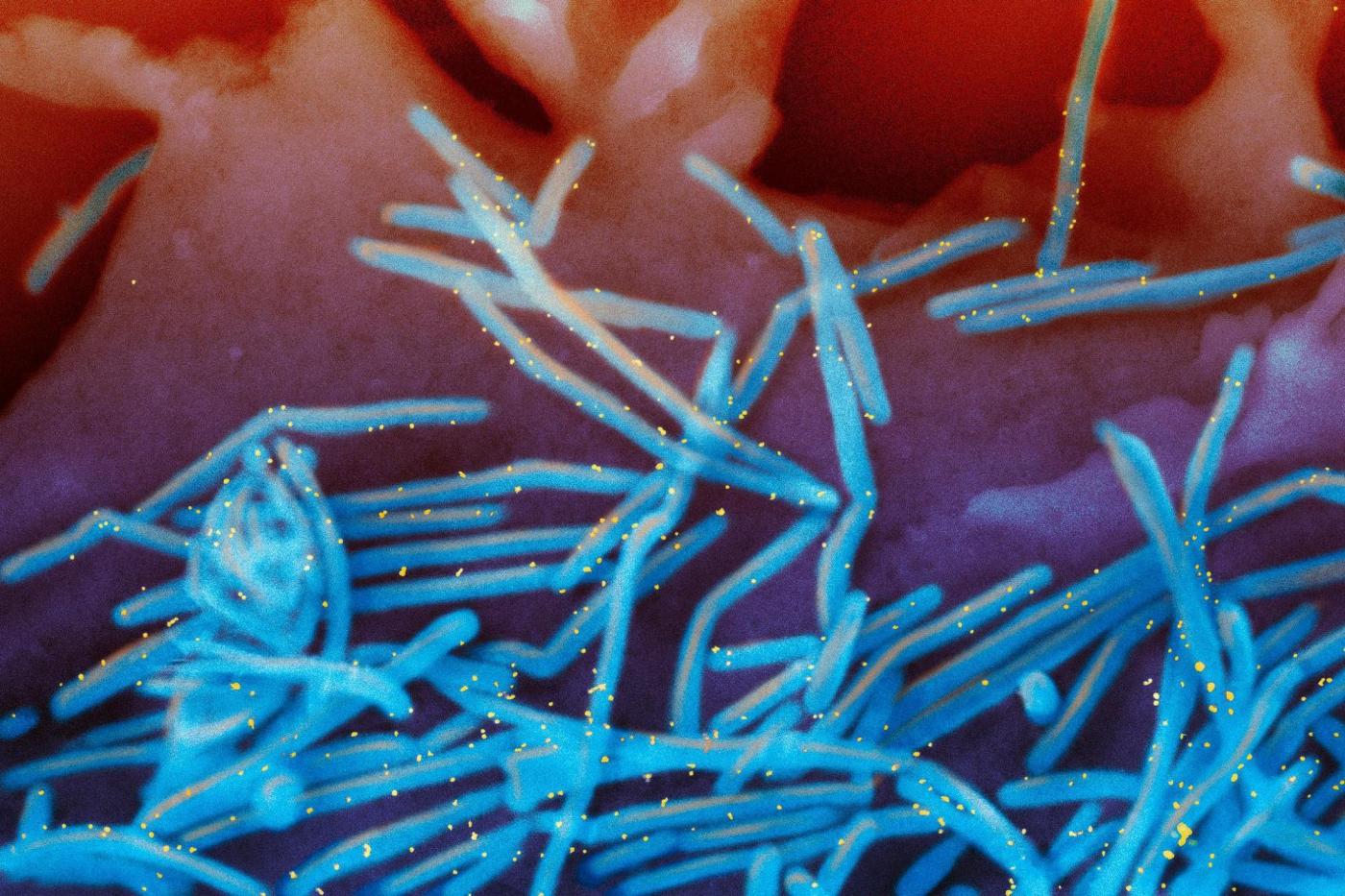
Among the strains of concern is the A H3N2 virus, which has a historical pattern of causing significant hospitalizations and fatalities, particularly among older adults. Current data indicates that this subtype is the most frequently reported this season, with a concerning 89% of the analyzed H3N2 infections comprising a new variant, known as the subclade K variant. This variant differs from the strain included in this year’s flu vaccines, leaving experts apprehensive about its potential impact.
Flu seasons often peak in February, meaning it is premature to assess the full implications of this vaccine mismatch. The CDC recommends annual vaccinations for everyone aged six months and older, noting that it is still not too late to receive the flu shot. As of now, about 42% of U.S. adults and 41% of children have received their flu vaccinations this season.
RSV and COVID-19: Trends and Vaccination Efforts
Respiratory syncytial virus (RSV) is another respiratory illness warranting attention, particularly due to its potential severity in infants and the elderly. Historically, RSV peaks in December or January, but this year’s cases are reported to be lower than usual at this point in the season. Dr. Cameron Wolfe, an infectious disease expert at Duke University, anticipates an increase in RSV cases, particularly in southern and mid-Atlantic states.
In response to this concern, new vaccines for RSV have been licensed for pregnant women and older adults, alongside laboratory-made antibodies for infants. As of October, approximately 41% of Americans aged 75 and older are vaccinated against RSV, while 40% of infants are reported to have protection.
COVID-19 activity remains relatively low, with the CDC indicating a decline from summer peaks. Recent research suggests that COVID-19 vaccines are effective in preventing severe illness among children, with a preliminary effectiveness rate of 76% for children aged nine months to four years. Despite this, vaccination uptake has been low this season, with only 7% of children and 15% of adults receiving the latest COVID-19 vaccine.
The CDC’s recommendation for COVID-19 vaccinations has shifted, now leaving the decision to patients. This change follows a broader trend of hesitancy, particularly in light of the previous administration’s leadership decisions regarding public health policies.
As winter progresses, health officials continue to monitor these respiratory viruses closely, advocating for vaccinations while preparing for potential increases in cases and hospitalizations. The coming months will be critical in determining the severity of the ongoing winter virus season.